Recent Posts
Patient recovering after COVID-19 hospitalization, extracorporeal membrane oxygenation support

Since the COVID-19 pandemic began, medical professionals have stressed that older adults had an increased risk of serious disease or hospitalization. Although COVID-19 tends to be mild for some, it still carries the risk of causing life-threatening lung failure. even in young, previously healthy people. An example of that is Juan Pablo Nunez, who goes by J.P.
J.P. is a busy and healthy 23-year-old manager at his family's restaurant in Eau Claire, Wisconsin. In September, he spent a late summer day learning to wakeboard on Lake Wissota in Chippewa Falls, Wisconsin. "I fell a lot, so I drank a lot of water," he says with a laugh. "After that, I felt very congested and started getting a fever."
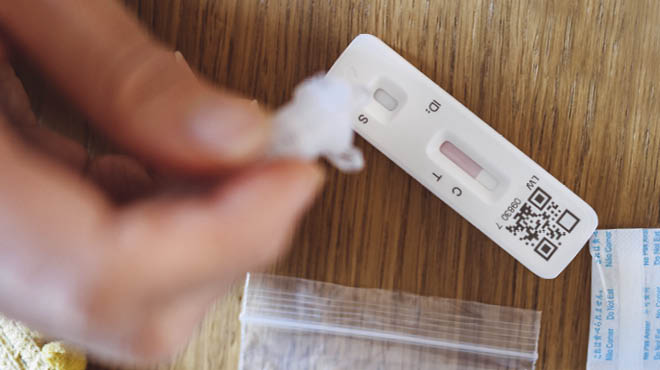
He was tested for COVID-19, and his results came back positive. J.P. managed his symptoms at home for several days, but his condition quickly changed about one week after his diagnosis.
"I woke up with 105 F temperature and was having a hard time breathing," says J.P. "I couldn't stand up, so my girlfriend brought me to the ER."
That was the Emergency Department at Mayo Clinic Health System in Eau Claire. J.P. expected that he would be given supplemental oxygen and be sent home. Instead, the care team was concerned enough with his oxygen levels that he was admitted to the hospital.
"COVID-19 can cause tiny air sacs in the lungs, called alveoli, to fill with fluid, and this lowers the lungs' ability to provide vital organs with the necessary oxygen to function property," says Ali Zaied, M.D., a pulmonologist and critical medicine physician. "At first, Mr. Nunez needed a nasal cannula for oxygen support, which is consistent with many other patients with COVID-19. Then his condition progressed over the following days, and he required high-flow oxygen."
Five days after being admitted to the hospital, J.P. was transferred to the Critical Care Unit. Dr. Zaied used bilevel positive airway pressure to deliver pressurized air into J.P.'s lungs. Instead of improving, J.P.'s condition deteriorated further, and eight days after being admitted to the hospital, the care team talked with him about going on a ventilator. A ventilator pumps air into patients' lungs when they are unable do breath adequately on their own, as was the case with J.P.
His mom and girlfriend said goodbye to J.P. through the exterior window of his hospital room.
"I kept thinking there must be something else we could do, but there wasn't," says J.P. "It was really hard because I was worried about them, and they couldn't be with me."
Despite maximum oxygen support from the ventilator, J.P.'s condition did not improve. Dr. Zaied and the team consulted with their colleagues at Mayo Clinic in Rochester, Minnesota. They decided to transport J.P. to Mayo Clinic Hospital, Saint Marys Campus.
"Mr. Nunez had severe refractory hypoxemic respiratory failure, which means he was unable to maintain normal oxygen levels, even with heavy sedation, mechanical ventilation and prone positioning," says Kyle Bohman, M.D., a Mayo Clinic anesthesiologist who was part of the team that cared for J.P. "Extracorporeal membrane oxygenation support was required for his case."
With extracorporeal membrane oxygenation (ECMO), blood is pumped outside of the body to a heart-lung machine that removes carbon dioxide and sends oxygen-filled blood back to tissues in the body. Blood flows from the right side of the heart to the membrane oxygenator in the heart-lung machine, and then is rewarmed and sent back to the body.
Extracorporeal membrane oxygenation support is available at Mayo Clinic Health System in Eau Claire, but patients who require this level of support often are transferred to Rochester to keep limited local equipment available for heart surgeries or other procedures. J.P.'s family braced themselves for a long hospital stay.
"Our patients with COVID-19 who require EMCO support, and those at other ECMO centers across the nation, tend to require this level of intervention for one to eight weeks, with the average being around three weeks," explains Dr. Bohman.
To date, J.P. is the youngest patient whom required extracorporeal membrane oxygenation support for COVID-19 at Mayo Clinic in Rochester. While he doesn't remember being transferred to Rochester, he recalls feeling calm and knowing he was in good hands during that time.
After one week, J.P.'s condition had improved enough that he no longer required extracorporeal membrane oxygenation support, and he was able to go home to further recover and follow up with his local health care team.
"He happened to be on the short side of the distribution of ECMO runs. I think that his age helped him recover more quickly than others," says Dr. Bohman. "I can't help but think that luck was on his side too."
Dr. Zaied agrees. "He had a quick and remarkable course for someone on ECMO," he says. "He has some residual scarring on his lungs, but is back to about 95% functional capacity."
Four months after being hospitalized, J.P. reports that he tires more easily and occasionally is winded, but he is back to work.
"I really missed work. I didn't step into the restaurant for two months," says J.P. "My family has done so much for the past 20 years, and it has given me an amazing life. Now it is my turn to do my part to do what I can at the restaurant."
Reflecting on J.P.'s case, Dr. Zaied stresses that teamwork was critical to his success.
"Taking care of someone as sick as Mr. Nunez was a team effort, and that includes doctors, nurses, respiratory therapists and so many others. You need an entire group of providers who are dedicated to providing the best care possible," says Dr. Zaied. "He was memorable for many of the front-line staff because he was so young and so sick. Some of the nurses who cared for him have seen him at his restaurant and start crying. It's very emotional for them."
It's emotional for J.P., as well.
"I'm really thankful to all the staff. I don't remember all their names, but there are so many great people that I wish I could shake their hands and thank them," says J.P. "They saved my life, and for that, I will always be grateful."