Recent Posts
At-home COVID-19 tests: What to know about expiration dates, new variants
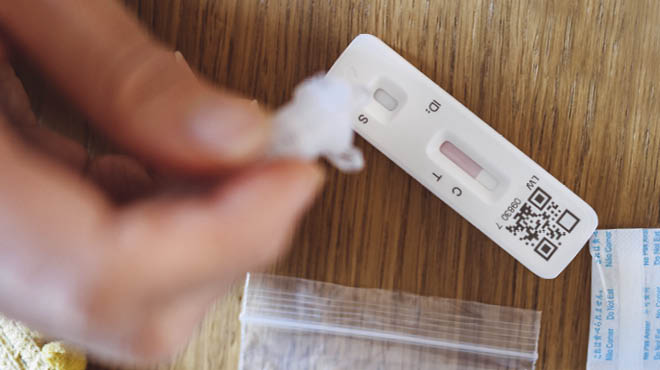
At-home COVID-19 kits allow you to collect samples and detect active COVID-19 infections. But what if you have at-home COVID-19 tests nearing expiration or expired on your shelf?
Companies arbitrarily set the original test dates because these diagnostic at-home tests were developed rapidly. So check your boxes before you toss them.
Now, 3 1/2 years into the pandemic, those manufacturers have had the opportunity to go back and assess the test performance over prolonged periods of time. And they've updated the expiration dates in many cases.
If you have tests at home, search the Food and Drug Administration website for information on updated expiration dates.
If you take a test that is beyond the expiration date and the test is positive, that's likely a reliable result, especially if you have a respiratory illness. If you get a negative result from a test beyond the expiration date, ensure the test doesn't have an extended expiration date. If it's beyond that expiration date, get another test or have a healthcare professional collect a swab for a lab-based test before you rule out COVID-19.
Can at-home tests detect current strains of COVID-19?
Yes, at-home tests should detect the currently circulating strains of COVID-19. The good news is that most of the changes in the virus with these new variants are in the spike protein, which is the part of the virus that binds to the cells. And the protein these antigen tests are looking for is a different protein where fewer mutations occur. So, that allows healthcare professionals to confidently say that these tests should pick up the circulating strains.
Testing positive
Are you contagious if you test positive for COVID-19? Yes, most likely you are. When an at-home antigen test is positive, that person still is shedding or excreting a high amount of viral protein. In most cases, that means that the person is shedding a high amount of virus, and likely a high amount of virus that could be spread from one person to another.
If you get a positive at-home antigen test, consider yourself at risk of spreading the virus to others.
Testing negative
Testing at home is recommended if you experience COVID-19 symptoms. If it comes back positive, you likely have a COVID-19 infection. But what if you have symptoms and the test comes back negative?
If your test comes back negative at home and you still have those typical symptoms of COVID-19, such as sore throat, cough, fever and body aches, that's when it's recommended that you go in to see your healthcare team and get a swab collected that can be sent to a lab for a PCR-based test. That will provide the most reliable information on whether you truly have or don't have COVID-19.
When should you test for COVID-19?
There are a few instances recommended for testing:
- If you develop symptoms, such as fever, cough, sore throat, runny nose or body aches.
- If you've spent time with someone with a confirmed diagnosis of COVID-19.
- If you plan on visiting someone at high risk of severe illness, including a person with cancer, an older adult or someone taking medications that suppress their immune system.
If you've been exposed to the virus, the recommendation is to wait a few days after exposure. Don't go home and take a test immediately because it won't have been enough time for the virus to reach levels that will trigger antigen tests to be positive. Wait three days after an exposure and then take a test.
If the test is negative, consider taking another test the following day or 48 hours from then. Typically, by day five after exposure, you're likely in the clear if you test negative.
Temperatures and at-home COVID-19 tests
Tests may be affected by fluctuating temperatures across geographic areas. If you're in an area that has experienced subzero weather or temperatures well above 100, as many parts of the U.S. have during the summer months, it's always a good idea to check the packet that comes with a test to look for acceptable storage conditions as determined by the FDA.
Matthew Binnicker, Ph.D., is the director of the Clinical Virology Laboratory at Mayo Clinic.





