Recent Posts
Advice from breast cancer survivor: 'Listen to your body'

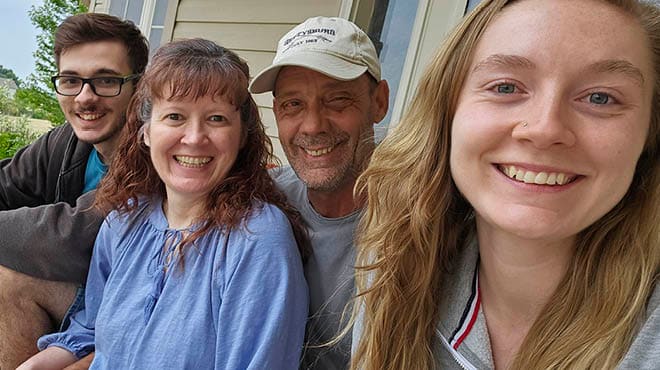
Kari Skaar knows the importance of asking the right questions. As a high school chemistry teacher, she has a curious and scientific mind, and isn't afraid to speak up when something doesn't seem right.
That's why she didn't wait to see her primary care provider when she developed severe breast pain in June 2019. Earlier in the year, the 44-year-old Bloomer, Wisconsin, resident discovered a cyst in her breast, but this time something felt different and she didn't want to wait to get it checked out.
"I assumed the cyst had gotten larger and needed to be aspirated," says Kari. "But breast pain isn't something one normally gets, so that was part of the reason I went in."
During her appointment with Brandi Zimmerman, a Family Medicine nurse practitioner at Mayo Clinic Health System in Bloomer, Wisconsin, she explained the breast pain and swelling she was experiencing.
"The pain was really bad. It felt like mastitis or a plugged milk duct," explains Kari.
Brandi sent Kari for an ultrasound the next day, which showed the cyst in addition to a larger mass that was not present in scans from earlier in the year. Kari's care team needed a biopsy of the new mass to make a diagnosis.
"I was freaking out," says Kari. "My husband (Phillip Skaar, M.D., a Family Medicine physician) called a friend of his from college who is an anesthesiologist in Eau Claire and asked for a recommendation. He said, 'Go see Dr. Appel.'"
That is Angela Appel, M.D., one of the general surgeons at Mayo Clinic Health System in Eau Claire, Wisconsin. One week later, Kari had an appointment with Dr. Appel, and her biopsy was scheduled.
"I was nervous but in a bit of denial," says Kari. "At the time, I was 43, and there is no family history of breast cancer. I figured it had to be something else because it just didn't make any sense."
Dr. Appel called Kari the day after her biopsy with her results.
"I was in the parking lot of the grocery store when she called and told me the biopsy showed cancer," says Kari. "I was devastated. That night, my parents were visiting. My mom was with me when Dr. Appel called. My husband was at work and knew that I was waiting for the phone call. I had to send him a text message telling him the results. That was very difficult. I didn't want to let the kids know right away. I wanted more information first. So that night, I tried to pretend like nothing was wrong. That was very hard."
Dr. Appel explains that breast cancer is not only a difficult physical diagnosis, but also a difficult emotional diagnosis for all women.
"Kari responded exactly like most women by feeling worried and upset. It's OK for women to grieve and be emotional during this time," she says.
Soon her entire family found out that Kari was diagnosed with stage 1B triple-negative breast cancer. She met with Sandeep Basu, M.D., a Mayo Clinic Health System oncologist, and Jill Depke, a Mayo Clinic Health System nurse practitioner in the Albert J. and Judith A. Dunlap Cancer Center at Mayo Clinic Health System in Eau Claire. Her multidisciplinary care team, including oncologists, radiologists, surgeons and pathologists, mapped out the treatment plan for Kari.
"First, Kari had chemotherapy with four cycles of Adriamycin and Cytoxan, followed by 12 weeks of Taxol," says Dr. Basu. "This is a fairly aggressive regimen and is considered the standard treatment for woman in her age group with this diagnosis."
To Kari's relief, chemotherapy started right away.
"I'm glad it happened quickly," she says. "I was finally doing something and not in limbo anymore."
Chemotherapy treatments
Kari received chemotherapy treatments in Eau Claire and found herself in a student role.
"The staff in the cancer center was phenomenal. Coming from a science background, I was very interested in the chemo, like where it comes from and how it works," says Kari. "I asked a ton of questions of the nurses because I wanted to be the student. Then when I went back to the classroom (at school), I could share what I had learned with the kids. The nurses answered every single question."
Kari was extremely fatigued after the chemotherapy treatments started, but she did not experience much nausea or sickness. Soon her hair began to fall out.
"I knew it was coming, but it happened sooner than I was expecting. When it started falling out, my head hurt like it does if you have a very tight ponytail," says Kari. "I started crying and my daughter came into the room and said: 'Mom, it's just hair. It will grow back.' She was right, and I got over it pretty quickly. As soon as I shaved it all off, I was fine."
A more significant setback that Kari experienced was blood clots. After her second round of chemotherapy, Kari began to notice a neck ache that spread to her ear. At first, her care team thought it was caused by muscle aches and bone pain due to medication she was taking, but soon the pain was tingling down her now-swollen arm. An ultrasound in the Emergency Department at Mayo Clinic Health System in Bloomer revealed that she had a blood clot in her arm. Kari needed three procedures in the Interventional Radiology Cath Lab in Eau Claire to "Roto-Rooter" her arm and a four-day hospital stay to clear her veins of this potentially serious complication.
By the end of September 2019, Kari was back teaching in the classroom. She taught Mondays through Thursdays, and then completed chemotherapy treatments each Friday.
"I asked to go back to work because I was feeling pretty good," says Kari. "I knew being busy and productive would help me mentally. My immune system also was in better shape after A/C (Adriamycin and Cytoxan chemotherapy) so I wasn't too worried about catching anything. There were days that I felt bad, but I went to work because I was able to do so. I wanted to be there."
"Kari took any setback in stride," says Dr. Basu. "After completing chemotherapy with an excellent response, she went on to have her surgery with Dr. Appel."
Surgery options
Kari had a single mastectomy surgery to remove her right breast in January.
"Most patients with breast cancer either have a lumpectomy or mastectomy. The decision rests on imaging findings and the size of the cancer compared to the size of the breast," says Dr. Appel. "For Kari, the size of the cancer meant that we could not perform breast-conserving therapy, also called a lumpectomy, so a single mastectomy was her best option."
There are many breast reconstruction options after a mastectomy for patients with breast cancer. Kari decided to not have breast reconstruction surgery after her procedure, but 54% to 63% of breast cancer patients do have some type of breast reconstruction procedure after a single or double mastectomy. After six months of chemotherapy, a mastectomy, MRI and positron emission tomography scans, and multiple appointments, Kari decided that she was not interested in reconstructive surgery at that time.
Kari developed a blood clot again after her mastectomy, so she was placed on blood thinners again. After a four-week recovery, she returned to her classroom and felt good enough to teach the rest of the year. She transitioned to virtual teaching four weeks later when the COVID-19 pandemic began.
Recovery and looking to the future
Today, Kari is cancer-free, feeling well and reflecting on her journey.
"I'm pretty much back to normal. Chemo put me into postmenopause, but overall I'm feeling good," she says. "I have my fingers crossed that it doesn't come back, but I'm not one to dwell on it. Plus worrying doesn't make it any better."
Dr. Appel isn't surprised with Kari's attitude.
"Kari is very grounded, and was extremely focused on moving forward during her treatment," she says. "She was strong and determined to keep her sights on the long-term goal the entire time."
And she continues to think long term, as she is planning a trip to Maui, Hawaii, in March 2021 with a friend to celebrate her cancer remission. The trip was originally planned for March 2020, but it had to be postponed due to the COVID-19 pandemic.
"When I think back, I almost didn't go in for the breast pain because I had a mammogram scheduled for the next month," says Kari. "I'm just thankful that I went in when I did because something didn't seem right. It's so important that women listen to their bodies and have things checked out."
Dr. Appel agrees.
"It's important that people be advocates for their own health," she says. "Kari was concerned about the changes she noticed in her body, sought care and spoke up when something didn't seem right. We want everyone to be empowered to manage their own health just like Kari."